Cardiometabolic diseases such as type 2 diabetes, obesity and coronary heart disease, which together are the leading cause of death worldwide, are still on the rise. Sufferers often have to take several medicines a day for years to maintain their health. In a research project funded by the European Union, scientists from six countries and more than 20 different institutions have now investigated how this affects both the disease and the gut.
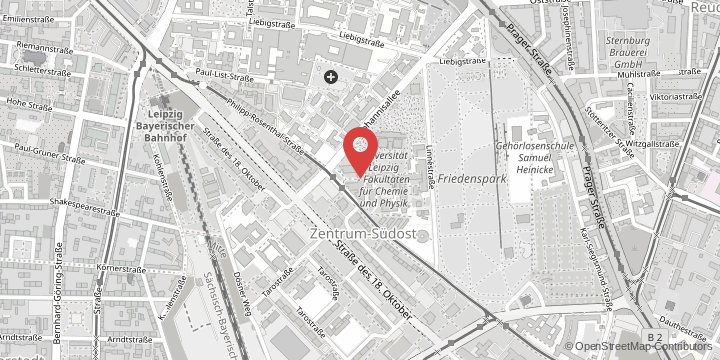
“For almost a decade of modern microbiome research, it was really rather naive of us to ignore the role played by drugs, which all pass through the gut. The importance of antibiotics was clear early on, and later that of metformin and statins. Now it has dawned on us that in principle all drugs may be able to chronically change the composition of our bacteria. We will never be able to ignore this finding in future analyses,” said Professor Stumvoll, head of the Department of Endocrinology, Nephrology, Rheumatology at Leipzig University Hospital.
In the recently published study in the renowned journal Nature, data from 2173 patients with cardiometabolic disease was analysed. The most important finding is that drugs can have a stronger influence on the composition of gut bacteria and on the metabolism of the host than disease, diet, and smoking combined. The extent of the observed changes also depended on the drug dose. In addition, the researchers found that many of the desirable, but also undesirable, effects of drugs in the body are achieved indirectly – through changes to the microbiome.
.
Making medical use of unexpected effects
The gut microbiome is made up of billions of microorganisms that live in our guts and are essential for the body to function normally. Recently, the microbiome has attracted a lot of scientific interest due to its sensitivity to disease. “However, studies examining the gut microbiome in relation to cardiometabolic health have generally not taken into account medication use. As such, it is unclear whether the described changes in the microbiome of patients are an expression of the disease or merely a reflection of the treatment. It is important to understand this if you want to use gut bacteria to promote health, or learn how exactly drugs affect the body,” said Dr Chakaroun, one of the study’s lead authors and a researcher and doctor at Leipzig University Hospital.
In the study, the researchers found that drugs taken at the same time can reinforce each other’s effect on the microbiome. Most of the medicines have a positive effect. For example, it was shown that the simultaneous administration of beta blockers and diuretics, both classes of drugs used to treat high blood pressure, is associated with an increasing number of bacteria of the genus Roseburia in the intestine. These bacteria have an anti-inflammatory effect in the body by breaking down dietary fibre and producing short-chain fatty acids from it, which protect against inflammatory processes. Such unexpected effects of drugs could be used for medical purposes in the future.
Repeated antibiotic use limits gut microbiome diversity
The study also points to potentially harmful effects of repeated antibiotic use, which has increased in recent decades. In patients who had taken antibiotics several times, the team found that the gut microbiome had become less diverse, more closely resembling a disease-like state. However, it is also possible that patients who need to take more antibiotics are predisposed to develop cardiometabolic disease and that this relationship is actually modulated by a common denominator in the immune system. Antibiotics should, however, still be taken if this is deemed necessary following an appropriate medical assessment; the medical community has long since understood that antibiotics should only be used efficiently and economically based on strict indications.
Original title of the publication in Nature:
“Combinatorial, additive and dose-dependent drug–microbiome associations”, Doi: 10.1038/s41586-021-04177-9